Coalition Policy Priorities
Here are the Coalition's Priorities to Support Individuals with Autism Spectrum Disorder (ASD), Developmental Disabilities (DD), and Mental Health conditions (MH) in accessing Behavioral Health services, including ABA services.
Medicaid Coverage Accessibility Challenges
Most Illinois Families with Medicaid Insurance are waiting to Access ABA Services for their children with ASD. What specifically is stopping families from getting access to ABA today?
Currently, most ABA providers cannot find the licensed professionals Medicaid requires to supervise the behavior analyst (BCBA) they employ. This is leaving families on very long wait lists with most families not finding any approved Medicaid ABA providers in their communities. The behavior analyst is the most common practitioner type that oversees ABA therapy and within commercial employer-based insurance, there is no requirement for them to be supervised. Unfortunately, there is a workforce shortage in all human services industries, and it is very difficult to find the required licensed professionals.
Learn more about access challenges in Medicaid plus a Call To Action!
Adult Services for ASD/ID/DD offering access to ABA Services.
Adults should have access to behavioral health treatments throughout adulthood based on their individual needs, be based on medical necessity, and not be constrained by age. Our Coalition supports individuals and providers when attempting to authorize ABA therapy for adults through health insurance. We also support utilizing ABA principles in adult services such as behavior support services in waivers and adult day services.
New Illinois Law strengthens the use of ABA Therapy's Generally Accepted Standards of Care (GASC) in Medical Necessity Determinations for treatment services for ASD/DD/MH.
The U.S. Health and Human Services defines GASC as standards grounded in evidence-based medicine, widely accepted best clinical practice or criteria issued by recognized professional medical associations, accreditation bodies, government agencies, or other nationally recognized healthcare quality organizations. Link to read more
On the state level, newly passed legislation expanded access to quality and reliable insurance for mental healthcare. HB 2595 requires every insurer to provide coverage to all medically necessary mental healthcare across the state. This includes the treatment of mental, emotional, nervous, or substance use disorders starting January 1, 2023. The bill establishes a clear definition and standards for when services and treatment qualify as medically necessary.
Here are the Four Generally Accepted Standards of Care (GASC) we expect to be used in medical necessity determinations for authorizing ABA therapy in the treatment of ASD/ID/DD:
- Applied Behavior Analysis Treatment of Autism Spectrum Disorder: Practice Guidelines for Healthcare Funders and Manager.
- Council for Autism Service Providers (CASP) (2020).
- The Model Coverage Policy, (GASC)
- ABA Coding Coalition (2022).
- Clarifications Regarding Applied Behavior Analysis Treatment of Autism Spectrum Disorder: Practice Guidelines for Healthcare Funders and Managers (2nd ed.)
- Behavior Analyst Certification Board® (BACB®) (2019).
- DSM-V, Diagnostic and statistical manual of mental disorders (5th ed., text rev.)
- American Psychiatric Association. (2022).
Network Adequacy Concerns to Ensure Adequate Provider Networks to Meet Consumer Needs
This would include supporting individuals who need more intensive treatment with additional technician staff to ensure health and safety, get access and authorization approval for the level of care needed.
Continuing to apply the state's Mental Health Parity law and New Legislation supporting Standards for Medical Necessity into ABA Service Authorizations
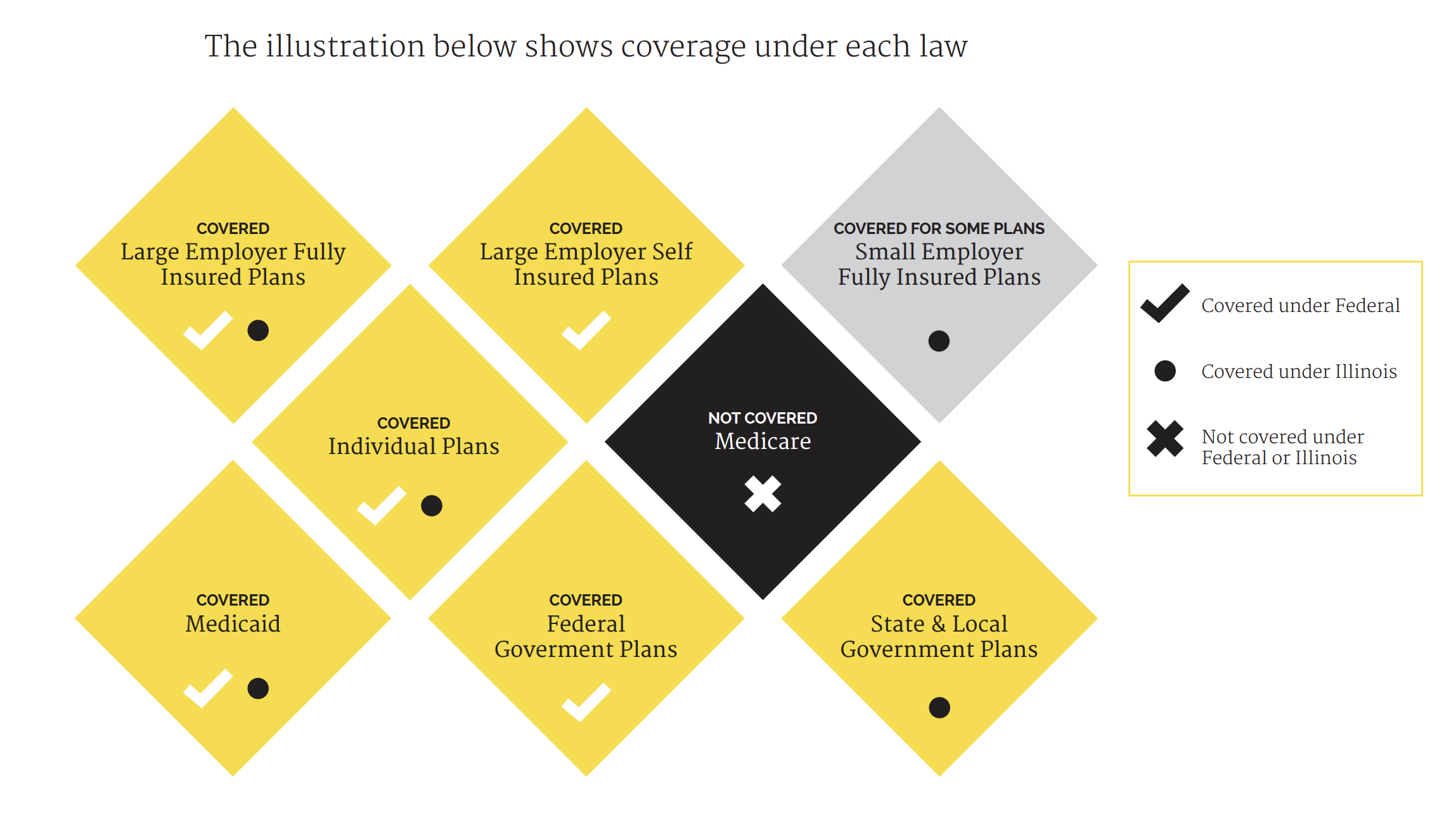
Illinois enacted a new parity law within Public Act 99-480 on September 11, 2015, to advance parity
implementation and expand on the Federal law. The law strengthened parity by including requirements for consumer education, more plans covering mental health and addiction services, and applied parity to additional health plan types at the state level. As discussed above, HB2595 offered clear definitions and standards for when services and treatment qualify as medically necessary.
Source: https://thekennedyforumillinois.org/wp-content/uploads/2015/12/Summary-of-HB-1-Parity-Provisions.pdf
PLEASE SHARE YOUR STORY WITH US!
Our purpose is to gather information about successes and challenges in accessing treatment.
As you share your story, the Coalition will tabulate them into data and monitor how benefits and systems are supporting Illinoisans with autism, developmental disability, and mental health disorders in getting access to ABA. We will share our data and stories with stakeholders to educate and influence public policy to continue our efforts to assure everyone is getting access to the treatments and support they need. The Coalition will keep all personal information confidential.
