Coalition Policy Priorities
Here are the Coalition's Priorities to Support Individuals with Autism Spectrum Disorder (ASD), Developmental Disabilities (DD), and Mental Health conditions (MH) in accessing Behavioral Health services, including ABA services.
New Behavior Analysts Licensing Act
Now that licenses have rolled out for behavior analysts, it is time to focus on learning how much staff time and cost ABA providers will incur to come into compliance with the CPOM/Ownership requirements found in the Licensure Act, and how we will forge ahead. CPOM stands for Corporate Practice of Medicine. Providers participating in the Coalition will have access to the webinar recording. Learn more about joining the Coalition at https://ilasd.com/about/. Are you an ABA provider organization? if so, follow this link to register for the CPOM training.
__________________________________________________________________________________________________________________________________________________________________
Medicaid Coverage Accessibility Challenges
Most Illinois Families with Medicaid Insurance are waiting to Access ABA Services for their children with ASD. What specifically is slowing down families getting access to ABA today?
Board Certified Behavior Analysts (BCBA) are now licensed practitioners in the state and can deliver ABA therapy. This has opened up service access for many families. However, we still have an extreme shortage of approved Medicaid providers to deliver ABA services, which leaves families on long wait lists for services. ABA stands for Applied Behavior Analysis, and within the Medicaid coverage, it is known as Adaptive Behavior Services. Our Coalition is working with the state Department of Medicaid (HFS) to reduce providers' barriers to delivering treatment. Barriers include a requirement for Registered Behavior Technicians, the care staff who deliver direct treatment. Our Coalition believes that behavior technicians who have completed the rigorous training and proven their competency in delivering ABA services should become billable at that point. Then, the Technician can take the test and complete their certification to become a Registered Behavior Technician (RBT). This change would get many families off the waitlist and into services much quicker. Another challenge for providers delivering ABA therapy is low reimbursement. Our Coalition worked with HFS to increase reimbursement rates back in 2021, but unfortunately, with inflation and workforce shortages in all human services industries, maintaining services is difficult.
RBT Medicaid Update May 2025: We have been meeting with HFS over the past six months on a consistent basis, and we have been very pleased with their involvement and flow of conversations. We believe they will lift the requirement of RBT for the first 120 days of employment. We will have more on this soon!
______________________________________________________________________________________________________________________________________________________________
Long waitlist for Autism Diagnostic Evaluations is leaving families without therapies.
Most families report an eight to twelve months waitlist for psychological evaluations for Autism Spectrum Disorders (ASD). Our Coalition is advocating for expanding the licensed practitioners who can screen or diagnose for ASD. It is key that the child with suspected ASD gets access to therapies and treatments right away.
For diagnosing practitioners, currently psychologist and developing pediatricians, we are hoping to see the following practitioners added to complete an ADOS which is a common testing tool for ASD: Licensed social workers, clinical professional counselors, school psychologists and master’s level school psychologists supervised by a school psychologist, certified psychiatric nurse practitioners, certified nurse practitioners, and primary care physicians.
For autism screenings, we advocate that primary care physicians and other practitioners, such as nurse practitioners, in primary care settings be able to complete standardized autism-specific screening tools.
If an ADOS or autism-specific screening tool indicates signs of autism and the family is given behavioral treatment or ABA recommendations, we believe ABA treatment should begin as long as the child is on a waitlist for a more formal, comprehensive diagnostic evaluation (CDE).
Update May 2025: We would like to praise HFS for their understanding that requiring a re-diagnosis every 2 years is a hardship on families and for the diagnosticians. We hope to see HFS issue guidance on this soon! We have also been speaking with commercial or employer-based insurers regarding this challenge and with government agencies, encouraging them to expand the allowed practitioners who can diagnose or provide a preliminary diagnosis, so children can get into therapies sooner and then allow them to wait on a long waitlist for a more formal, comprehensive diagnostic evaluation.
_______________________________________________________________________________________________________________________________________________________________
Adult Services for ASD/ID/DD offering access to ABA Services.
Adults should have access to behavioral health treatments throughout adulthood based on their individual needs, be based on medical necessity, and not be constrained by age. Our Coalition supports individuals and providers when attempting to authorize ABA therapy for adults through health insurance. We also support utilizing ABA principles in adult services such as behavior support services in waivers and adult day services.
New Illinois Law strengthens the use of ABA Therapy's Generally Accepted Standards of Care (GASC) in Medical Necessity Determinations for treatment services for ASD/DD/MH.
The U.S. Health and Human Services defines GASC as standards grounded in evidence-based medicine, widely accepted best clinical practice or criteria issued by recognized professional medical associations, accreditation bodies, government agencies, or other nationally recognized healthcare quality organizations. Link to read more
On the state level, newly passed legislation expanded access to quality and reliable insurance for mental healthcare. HB 2595 requires every insurer to provide coverage to all medically necessary mental healthcare across the state. This includes the treatment of mental, emotional, nervous, or substance use disorders starting January 1, 2023. The bill establishes a clear definition and standards for when services and treatment qualify as medically necessary.
Here are the Four Generally Accepted Standards of Care (GASC) we expect to be used in medical necessity determinations for authorizing ABA therapy in the treatment of ASD/ID/DD:
- Applied Behavior Analysis Treatment of Autism Spectrum Disorder: Practice Guidelines for Healthcare Funders and Manager.
- Council for Autism Service Providers (CASP) (2020).
- The Model Coverage Policy, (GASC)
- ABA Coding Coalition (2022).
- Clarifications Regarding Applied Behavior Analysis Treatment of Autism Spectrum Disorder: Practice Guidelines for Healthcare Funders and Managers (2nd ed.)
- Behavior Analyst Certification Board® (BACB®) (2019).
- DSM-V, Diagnostic and statistical manual of mental disorders (5th ed., text rev.)
- American Psychiatric Association. (2022).
Network Adequacy Concerns to Ensure Adequate Provider Networks to Meet Consumer Needs
This would include supporting individuals who need more intensive treatment with additional technician staff to ensure health and safety, get access and authorization approval for the level of care needed.
Continuing to apply the state's Mental Health Parity law and New Legislation supporting Standards for Medical Necessity into ABA Service Authorizations
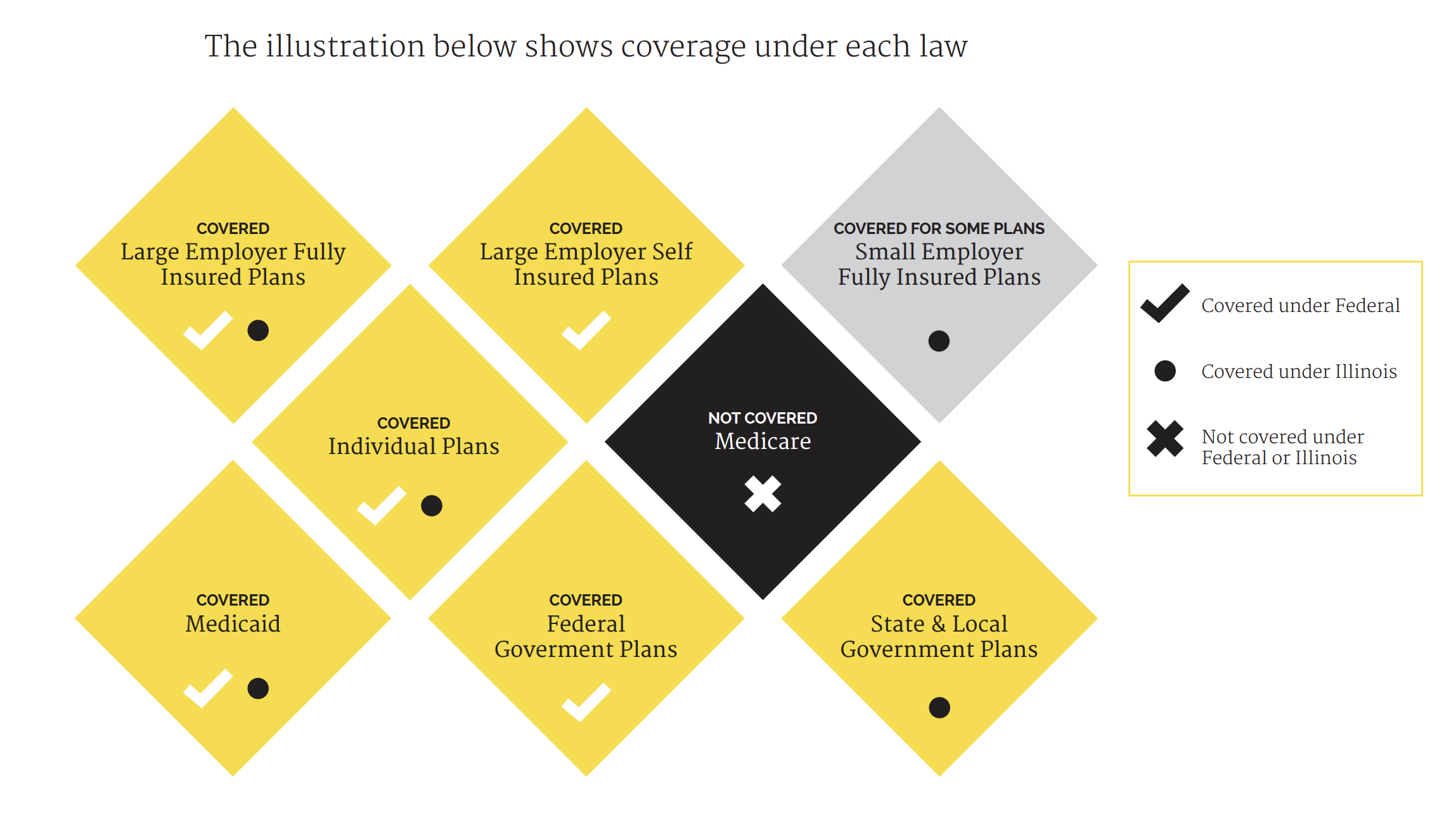
Illinois enacted a new parity law within Public Act 99-480 on September 11, 2015, to advance parity
implementation and expand on the Federal law. The law strengthened parity by including requirements for consumer education, more plans covering mental health and addiction services, and applied parity to additional health plan types at the state level. As discussed above, HB2595 offered clear definitions and standards for when services and treatment qualify as medically necessary.
Source: https://thekennedyforumillinois.org/wp-content/uploads/2015/12/Summary-of-HB-1-Parity-Provisions.pdf
PLEASE SHARE YOUR STORY WITH US!
Our purpose is to gather information about successes and challenges in accessing treatment.
As you share your story, the Coalition will tabulate them into data and monitor how benefits and systems are supporting Illinoisans with autism, developmental disability, and mental health disorders in getting access to ABA. We will share our data and stories with stakeholders to educate and influence public policy to continue our efforts to assure everyone is getting access to the treatments and support they need. The Coalition will keep all personal information confidential.
