Autism Insurance
Navigating Your Health Insurance Benefits and Coverage

The Health Insurance Process to Authorize ASD Treatment Services

Patient Protections – Parity, ACA, ERISA, Mandates, and More

ABA Therapy Authorization & Medical Necessity

Finding My Type of Health Insurance
Plan
The Health Insurance Process to Authorize Services
Autism Spectrum Disorder (ASD) is a condition listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM–5). Medical (medications) and behavioral treatments focus on treating the three core deficits of ASD: communication, social interaction, restrictive and repetitive behaviors (RRBs), interests, and activities. The intention of the treatment is to rehabilitate towards an end to intensive treatment and move to maintenance-type treatments such as Focused ABA, counseling or other services that support maintaining functioning or stabilization.
Medical Diagnosis, Prescriptions, and Recommendations
If you are seeking insurance coverage for treatment services for ASD, your individual will need a formal medical diagnosis (not a school diagnosis) resulting from the completion of psychological testing showing your individual scored in the range of ASD. A prescription from a physician or a recommendation on a psychological evaluation will need to state the type of treatment needed such as counseling, ABA or speech as examples.
Medical Necessity Criteria (MNC)
Individuals with ASD seeking insurance coverage for treatments will need to meet the medically necessary criteria for that particular treatment. “Medically necessary” means health care services, supplies, or drugs needed for the prevention, diagnosis, or treatment of your sickness, injury, or illness that follow the generally accepted standard of care for that diagnosis.
The term “medically necessary” generally refers to treatments that ameliorate (lessen) symptoms, manage symptoms, improve functioning, and/or prevent regression or deterioration. Elements of medical necessity include evidenced-based interventions or generally accepted treatments, goals to remediate deficits, signs and symptoms of the condition being treated, and treatment plans specifying frequency, intensity and duration of treatment that is considered to be clinically appropriate.
Specifically for ASD, the physician or psychologist will assess the patient’s needs and determine what treatment is medically necessary for the patient. The goal of the treatment is to ameliorate (to lessen) the patient’s symptoms, prevent self-injury, and challenging behaviors, and give the patient the best possible functioning condition to reduce current and future disability. The MNC is based on the ASD generally accepted standard of care (GASC). The ASD Practice Guidelines serve as the standard of care for ASD. You can read more about this at the CASP’s website at https://casproviders.org/asd-guidelines/.
Then, the insurer will also make a determination if the treatment prescribed meets the MNC for the ASD diagnosis. Unfortunately, some insurers use their own MNC that are more restrictive than the ASD Practice Guidelines mentioned above.
Denials, Appeals & Hearings
If the insurer issues a denial, the provider can request a “peer-to-peer review” which is a meeting with the insurer’s medical director to advocate for the patient’s need for treatment. If the insurer again denies the treatment, the patient or provider can file an “internal appeal” with the insurer and provide additional information or reasoning on why the patient should receive the treatment.
If the insurer continues to deny after the internal appeal, the patient or provider can then file an “external appeal” and the insurer will utilize a third-party reviewer. The patient or provider can also file a complaint with the insurer’s regulator.
A state hearing serves as the external review for Medicaid patients once they have exhausted the internal appeals process with the managed care plan.
Patient Protections: MHPAEA, ACA, ERISA, Mandate Law & Directive, and EPSDT
Mental Health Parity and Addiction Equity Act (MHPAEA, pronounced Ma-Pe-Ah)
Passed in 2008, MHPAEA is a federal law that ended discrimination against patients seeking mental health & addiction insurance services. The goal is for patients seeking mental health & addiction treatments to be treated the same as patients seeking medical and surgical treatments.
MHPAEA impacts most self-funded or fully insured employer-based health plans and Medicaid health plans delivered through a managed care plan.
The Federal Parity law’s mission is to stop the following from occurring to patients seeking MH/SUD services:
- Stop additional financial requirements, such as higher co-pays on mental health than medical co-pays.
- Stop patients from being forced to use out-of-network providers due to a lack of in-network providers.
- Stop the use of stricter medical necessity criteria than generally used by practitioners.
- Stop the over-burdensome prior authorization process.
- Stop requiring patients to try less intensive treatment “fail first” when a more intensive one was actually prescribed.
- Not allow age, visit or hour limitations that would not be equally applied to the medical/surgical care.
If a plan does not cover mental health conditions at all, it is not a MHPAEA violation. If the plan covers other mental health conditions and not ASD, that would be a violation.
The Affordable Care Act (ACA)
This law was signed into law in March of 2010 and required insurers to offer a robust, and comprehensive standard of coverage that all health plans authored after the start of the Act would have to provide. Healthcare advocates fought for uniform claim and appeal procedures including the requirement a plan provides a patient with the reason for a denial, a description of the standard or GASC used to deny care, and any new or additional evidence considered, relied upon, or generated by the plan in the course of denying a claim. The ACT also allows 180 days for the patient to file an appeal.
The ACA extended the protection of MHPAEA to individual health plans and small group/employer health plans by offering an Essential Health Benefits (EHBs) that requires mental health and addiction treatment benefit coverage by all non-grandfathered individual and small group health plans.
Section 1557 of ACA – Nondiscrimination statute. Section 1557 which prohibits discrimination on the basis of race, color, national origin, age, disability, or sex (including pregnancy, sexual orientation, gender identity, and sex characteristics), in covered health programs or activities. Speak directly to the health plan itself and not the employer if you suspect discrimination has occurred.
Section 1557 only impacts patients whose health providers receive federal health care dollars. If the health plan states it does not cover your disability and specifically singles out ASD for no coverage, the plan is violating the ACA because it is discriminating against people with ASD.
ERISA—Employee Retirement Income Security Act of 1974
ERISA is a federal law that establishes the rights of health plan participants, requirements of the health plan provisions, and funding and standards for the investment of health plan assets in self-funded employee health plans. ERISA provides specific protections for individuals appealing claim denials and establishes requirements for how a plan must review and respond to a claimant’s appeal. ERISA impacts self-funded and fully insured employer plans, except government plans.
ERISA requires the employer group plans to disclose the “summary plan description” document within 30 days of a request and the requirement of other documents related to the determination of medical necessity, denial reasoning and standards and references related to the denial.
Autism Mandate Law (commercial (private) plans only.
The “Autism Mandate” bill was passed late in December 2008. An insurance mandate requires state-regulated health plans to cover a defined benefit package passed by the legislation passed by the General Assembly and signed by the Governor. The state Act is 215 ILCS 5/356z.14.
The act impacted grandfathered health plans only, which could be either a Fully Funded Employer-Sponsored Group or an Individual and Family Broker Plan, all authored prior to the Affordable Healthcare Act. The Illinois Autism Mandate Law states children under the age of 21 will receive coverage for the diagnosis and treatment of autism spectrum disorders. The law also requires coverage for the following treatments: Psychiatric care provided by a licensed psychiatrist; Psychological care provided by a licensed psychologist; Habilitative or rehabilitative care such as counseling and treatment programs intended to develop, maintain, and restore the functioning of an individual, including Applied Behavioral Analysis (ABA); Therapeutic care, including behavioral, speech, occupational, and physical therapies addressing the following areas: Self-care and feeding, Pragmatic, receptive, and expressive language, Cognitive functioning, Applied behavioral analysis, intervention, and modification, Motor planning and Sensory processing. The Illinois mandate expanded for other diagnosis in 2009 though the Illinois Statue 215 amendment in 2009 added habilitative services for children less than 19 years of age with a congenital, genetic or early acquired disorder, including autism spectrum disorders. The state Act is 215 ILCS 5/356z.15.
The Illinois Department of Insurance offers an Autism Benefit FAQ.
With the patient protections under MHPAEA, the age cap, visit limit, and hours caps are quantitative treatment limitations and a violation under the MHPAEA law. We would argue that if the plan is subject to MHPAEA, then meeting medical necessity would be based on individual patient need and not based on age or the number of visits or hours already set in a plan. If the patient/individual receives a denial from the insurer because the clinical judgment (authorization request) from their treatment provider exceeds the coverage language for age, visits, or hours limits, an appeal needs to be filed based on the MHPAEA law.
Early, Periodic, Screening, Diagnosis, and Treatment (EPSDT) – Public Plans Only
Individuals with a Medicaid health plan and under the age of 21 have MHPAEA protections if receiving services through a managed care plan. They also have EPSDT protections.
The Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) mandate provides comprehensive and preventive healthcare services for individuals under age 21 who are enrolled in Medicaid. EPSDT is key to ensuring that individuals and adolescents receive appropriate preventive, dental, mental health, developmental, and specialty services.
The determination of whether a service is medically necessary for an individual must be made on a case-by-case basis and account for their particular needs. The state (or the managed care plan) should consider the individuals’ long-term needs, not just what is required to address the immediate situation. The state should also consider all aspects of an individual’s needs, including nutritional, social development, mental health, and substance use disorders.
ABA Therapy Authorization & Medical Necessity
ABA is delivered in two treatment models: Comprehensive ABA and Focused ABA. Social Skills Groups can also be provided.
“Comprehensive ABA Treatment” involves an intensity level of 30-40 hours of 1:1 direct treatment to the client per week, plus caregiver training and supervision. Comprehensive ABA treats multiple affected developmental domains, such as communicative, social, cognitive, emotional, and adaptive functioning. This intensive behavioral intervention also treats maladaptive behavior (actions that prevent people from adapting, adjusting, or participating such as noncompliance and tantrums) and restrictive and repetitive behaviors (repetitive or ritualistic movement, interests, and activities.) For some, a focus may be on closing the gap in their level of functioning with their typically developing peers.
“Focused ABA Treatment” generally ranges from 10-25 hours of direct treatment to the client plus caregiver training. Focus ABA targets a few challenging behaviors or key functional skills needing treatment.
Both comprehensive and focused ABA can be delivered in group environments.
“Social Skills Groups” are also part of ABA Treatment. If your health plan includes ABA coverage, it also includes social skills group coverage. Each client in the group has an individualized treatment plan with goals to treat ASD symptoms, specific to the client. Each individual in the group is billed for ABA, using a specific medical code identified for group services.
ABA is usually designed and supervised by a Board Certified Behavior Analyst (BCBA). BCBAs complete an assessment to determine maladaptive and restrictive or repetitive behaviors and skill abilities and deficits. The findings of the assessment are used to develop a treatment plan based on the results of the assessment. The BCBA also determines the dosage or level of intensity for treatment which will result in treatment hours per week. Behavior Technicians (BT) or Registered Behavior Technicians (RBT) are the direct care staff that delivers the treatment plan protocol under the supervision of the BCBA.
The American Medical Association (AMA) has medical codes called “Adaptive Behavior Assessment and Treatment Services” for the medical delivery of ABA therapy.
Authorizing “Assessment Services” in ABA Therapy with the Insurer
Once you have connected with a service provider, such as a behavior analyst, they will ask for your prescription or recommendation for treatment. They will work through their admissions process to determine if they can meet the needs of the patient.
Next, they will submit an authorization request to the insurer for “assessment services.” If the insurer authorizes (approves) the assessment service, the provider will observe and assess the patient, review the psychological testing results and diagnosis, and interview the parent, guardian, caregiver, and other service providers.
Authorizing “Treatment Services” in ABA Therapy with the Insurer
The provider will write a treatment plan based on the results of the assessment. The treatment plan and assessment results will be sent to the insurer requesting authorization for direct treatment services.
The insurer may authorize (approve) the treatment which means the treatment request meets medical necessity criteria. The authorization usually lasts six months for ABA therapy or a number of visits will be approved for other treatments.
The insurer may deny the authorization request if they determine the treatment does not meet MNC or the policy has no coverage for the treatment or ASD is excluded. The insurer will send the patient and provider an “adverse determination notice” (denial notice).
Types of Health Insurance Plans
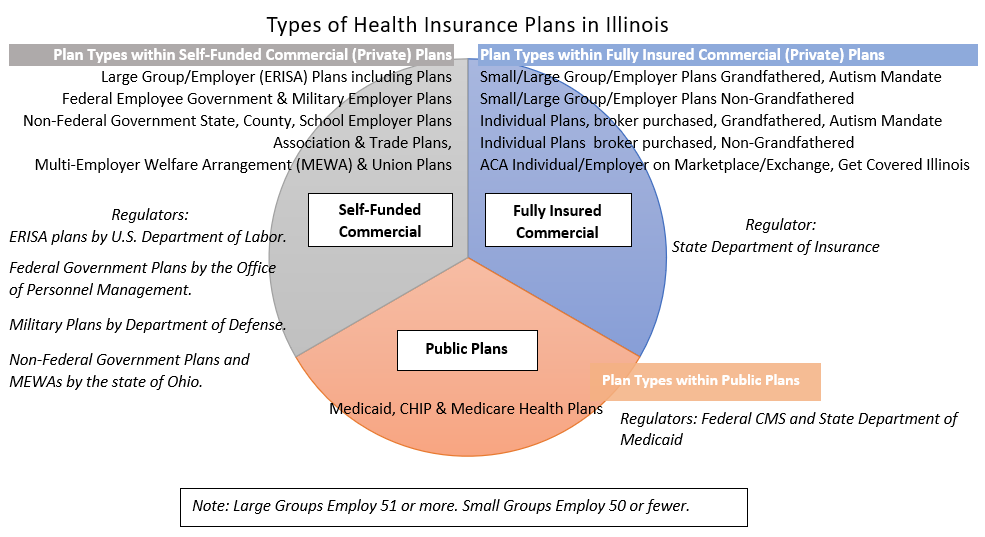
There are several different types of health plans sold in our state. Here are key questions to ask your insurer or HR department to help determine your type of health plan and the coverage in the plan.
- Is the health plan a commercial (individual or group/employer) plan (private) or a public plan?
- If a commercial plan, is the plan fully insured or self-funded?
- If employer-based, is it a large employer (> 50 employees) or a small employer (< 51 employees)?
- If the plan is a small employer or individual plan, is the plan grandfathered or non-grandfathered?
- Note: Grandfathered means the plan was authored prior to the start of the ACA and is not compliant with the ACA. Non-grandfathered means the plan was written after the start of the ACA and is ACA-compliant.
- Also ask for your health plan’s summary plan description or sometimes called evidence of coverage document to help you fully understand the plan’s coverages and exclusions for treatments.
Abbreviations: ASD (autism spectrum disorder), MNC (medical necessity criteria), GASC (generally accepted standard of care), ACA (affordable care act), ABA (applied behavior analysis), MHPAEA (federal mental health parity), Grandfathered (an older health plan without ACA protections)
This Guide was developed by Marla Root at Root Consulting, LLC for the Illinois Autism Insurance Coalition.
Reach out to us at help@ilasd.com or by calling 614-565-5765.
